Is there really such a thing as an arthritis diet? Dietitian Martin Lau answers this and other popular diet and nutrition questions
 Diet is a minefield for most of us but it can be even more mind-boggling when you have arthritis. What’s good? What’s bad? Are there really arthritis ‘superfoods’?
Diet is a minefield for most of us but it can be even more mind-boggling when you have arthritis. What’s good? What’s bad? Are there really arthritis ‘superfoods’?
Martin Lau is a dietitian and nutritionist who works for the charity Arthritis Action. He is a registered dietitian with the Health and Care Professions Council and offers nutritional consultations at Eastbourne and Harley Street.
Martin has kindly answered some of our questions – and he also agreed to answer some of yours. We put a shout-out on Twitter and Facebook, and the most popular questions are answered by Martin below.
Martin says: Despite what popular media suggests, there is no such thing as an arthritis diet. Healthy eating with a good variety from our main food groups is the foundation.
Martin says: Studies have found Omega-3 fatty acids may be beneficial to patients with arthritis. Also antioxidants and carotenoids from fruits and vegetables could dampen the inflammatory process. Vitamin D is also important too, especially for RA. However we should focus more on the whole dietary intake rather than individual nutrients.
Martin says: This is a fascinating area! For the majority of patients, no foods should be avoided. Food elimination could lead to nutritional deficiency and possible malnutrition for those with rheumatoid cachexia (weight loss due to losing muscle mass in people with rheumatoid arthritis). But there are a small group of patients who may ‘react’ negatively with certain foods.
My advice is to chat with your GP or your rheumatologist and possibly a referral to a dietitian for further investigation. Of note, Arthritis Action is a membership charity that offers dietetic support.
Martin says: From clinical studies the Mediterranean diet and vegetarian/vegan diet have been found to be beneficial to patients with RA. But some may not find them useful. Following a balanced and sensible eating regime is key. For osteoarthritis and gout, a weight-reducing eating regime, if overweight, is important.
Martin says: Garrett et al (1993) found up to 70% of patients believe that food affects their arthritis. But looking at present published evidence, the so-called ‘trigger foods’ seem unlikely to exert any significant effect on the course of arthritis.
On the other hand it does exist in a subgroup of patients. A study conducted by Dr Gail Darlington and her colleague in 1993 did find some culprit food in a very small group of subjects with RA. These foods varied from one individual to the other.
If you suspect food may be the cause of your arthritis symptoms, please speak to your GP or your rheumatologist.
Martin says: Drs Louise Goff and Mary Barasi (1999) looked at a local support group in Wales and found that 50% of subjects used supplements for their rheumatoid arthritis. But unless you have deficiencies or are unable to absorb nutrients, there is no robust evidence to suggest that vitamin and mineral supplements are effective in any type of arthritis. Always food first! If you are unsure whether you have any nutrient deficiencies, a nutritional assessment conducted by a dietitian would be useful.
There are a few joint-specific supplements widely available in health food stores and supermarkets. Glucosamine is a popular one. This amino sugar compound exists in two forms: glucosamine hydrochloride (GH) and glucosamine sulphate (GS). The results from clinical trials on GH is not convincing whilst GS demonstrated a mixed effectiveness. The current (2014) osteoarthritis management guideline published by the National Institute of Care and Excellence (NICE) stated ‘do not offer glucosamine or chondroitin products for the management of osteoarthritis’ due to the poor and conflicting evidence.
Cod liver oil is another popular supplement used by people with arthritis. As mentioned above, there is some evidence to support the use of Omega 3 fatty acids for arthritis. Key points I would like to highlight are:
- There is a difference in the Omega 3 fatty acid content between fish liver oil and fish body oil. The latter has more of these essential fatty acids.
- In order to meet the dose found to be effective, you will need to intake 2.7g of Omega 3 fatty acids per day (Arthritis Research 2014). Therefore lots of fish liver oil needs to be taken to meet this ‘therapeutic dose’, which could have serious side-effects (see the next key point).
- Fish liver oils also contain fat soluble vitamins such vitamin D and vitamin A. It is important to point out that large intake of vitamin A can cause serious side effects, particularly during pregnancy.
If you are going to use a fish liver oil supplement, consider a product with a high amount of Omega 3 fatty acid (in the form of EPA and DHA).
If you are interested in learning more about some of the popular supplements use for arthritis, Arthritis Research published a booklet which you may find useful.
Disclaimer: Please inform your GP and pharmacist before you take any supplements or other natural remedies. Do not attempt food exclusion or elimination without medical supervision.
Martin says: Eating healthily, by definition, is eating a balance and a variety of foods in all the food groups (carbohydrate, fruit and vegetables, meat plus meat products, dairy plus dairy products and oil plus fats), in order to provide energy and maintain health. All foods contain calories and overeating (even nutritious food) can contribute to weight gain. A reduction of calories intake is an important part in weight loss.
But, I do not like counting calories as this method can be very confusing! My key advice is to look at the portion size of meals.
Here are two ways you can reduce food intake by being more aware of portion sizes whilst eating sensibly:
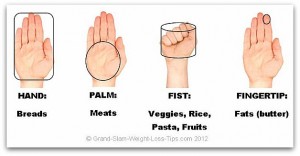
This is my favourite as you can visualise food portions simply by using the hand.- Portion Size Your Plate
Also, keeping a food diary helps to track daily food intake. Some of my weight management patients were surprised by how much they eat during the day. In order to lose and to keep weight off, a change in lifestyle is paramount.
Martin says: There is no special dietary regime for palindromic rheumatism. Healthy eating remains the sound foundation for inflammatory arthritis. A trial published in 2000 by the medical journal Clinical and Experimental Rheumatology, with a small subject number, found certain foods triggered an attack. However the authors’ conclusion was to assess each patient individually.
Martin says: Here are a few practical tips that could help:
- Use a bigger dinner plate. After all increasing the portion size of meals is a good way to get the calories in.
- In between meals include snacks such as nuts or yoghurts.
- Avoid reduced calorie foods.
- Use oil (such as olive or rapeseed) generously, especially using it as a salad dressing.
- Drink a mug of Horlicks or hot chocolate made with full-fat milk before bed drink.


